HYPERTHYROIDISM
-
Introduction
-
Clinical Signs
-
Diagnosis
-
Treatment
-
Photos
<
>
Hyperthyroidism is a disease caused by the overproduction of thyroid hormone, known as T3 and T4, from the thyroid glands in the neck. This hormone regulates the rate of chemical processes in a pet’s body. All animals can develop this disease, but the middle- to older-aged cat is the pet most commonly affected.
In most cases, increase in thyroid hormone with enlargement of the thyroid glands is caused by a tumor called an adenoma, which is not cancerous. In rare cases, hyperthyroidism is caused by malignant tumors known as thyroid adenocarcinomas.
Elevated levels of thyroid hormones stimulate a faster heart rate and a stronger contraction of the heart muscle. Over time, cats with hyperthyroidism may develop an enlargement and thickening of the left ventricle of the heart. If hyperthyroidism is untreated, these changes will eventually compromise the normal function of the heart and can result in heart failure. This means that some cats with hyperthyroidism will need additional treatment to control secondary heart disease. Once the underlying hyperthyroidism has been controlled, the cardiac changes will sometimes improve or may even resolve completely.
High blood pressure (hypertension) is another potential complication of hyperthyroidism and can cause additional damage to several organs, including the eyes, kidneys, heart, and brain. If hypertension is diagnosed along with hyperthyroidism, drugs may be needed to control the blood pressure and reduce the risk of damaging other organs. As in the case of heart disease, after the hyperthyroidism has been successfully treated, the high blood pressure will often resolve, and permanent treatment for it may not be required.
In most cases, increase in thyroid hormone with enlargement of the thyroid glands is caused by a tumor called an adenoma, which is not cancerous. In rare cases, hyperthyroidism is caused by malignant tumors known as thyroid adenocarcinomas.
Elevated levels of thyroid hormones stimulate a faster heart rate and a stronger contraction of the heart muscle. Over time, cats with hyperthyroidism may develop an enlargement and thickening of the left ventricle of the heart. If hyperthyroidism is untreated, these changes will eventually compromise the normal function of the heart and can result in heart failure. This means that some cats with hyperthyroidism will need additional treatment to control secondary heart disease. Once the underlying hyperthyroidism has been controlled, the cardiac changes will sometimes improve or may even resolve completely.
High blood pressure (hypertension) is another potential complication of hyperthyroidism and can cause additional damage to several organs, including the eyes, kidneys, heart, and brain. If hypertension is diagnosed along with hyperthyroidism, drugs may be needed to control the blood pressure and reduce the risk of damaging other organs. As in the case of heart disease, after the hyperthyroidism has been successfully treated, the high blood pressure will often resolve, and permanent treatment for it may not be required.
Hyperthyroid cats usually develop a variety of signs, which start subtly and become more severe as the disease progresses. The most common clinical signs of hyperthyroidism are decreased weight with increased appetite, thirst, and urination. Hyperthyroidism may also cause vomiting, diarrhea, panting, increased shedding, greasy or matted coat, rapid breathing, aggression, and hyperactivity.
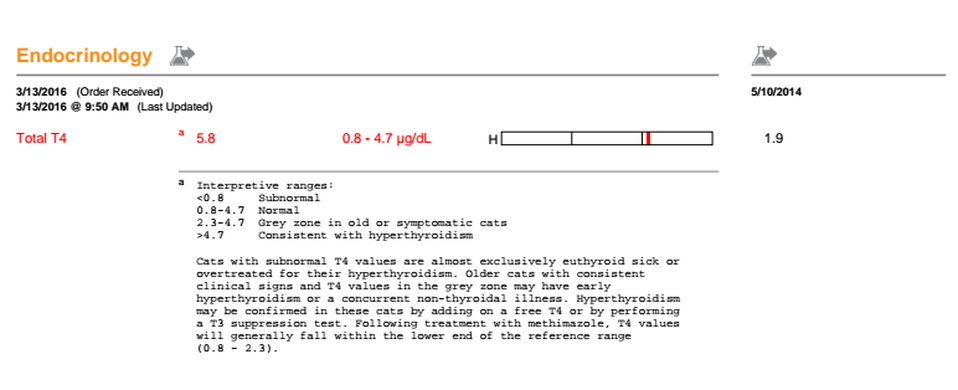
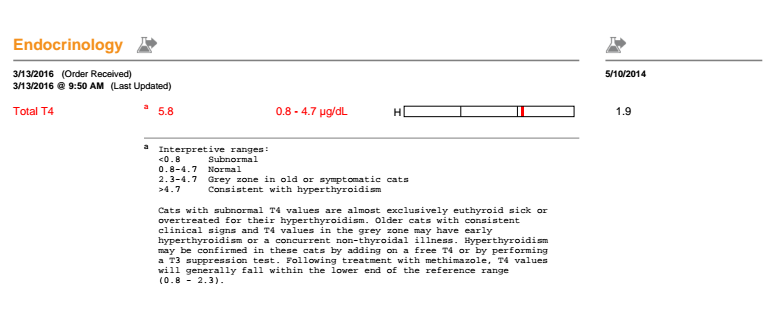
During
the physical examination, your cat's neck will be felt to check for enlarged
glands. Your cat's heart rate and blood pressure may also be checked. If
thyroid disease is suspected, your veterinarian will order a blood-chemistry
panel, a complete blood count, a thyroid hormone level, and a urinalysis.
Because the signs of feline hyperthyroidism can overlap with signs of kidney disease, liver disease, and cancer (especially intestinal lymphoma), it is important to perform the blood and urine diagnostics to confirm hyperthyroidism and to help rule out other conditions.
If concurrent heart disease is diagnosed, chest x-rays (thoracic radiography) and an ultrasound of the heart (echocardiography) may be useful in assessing the severity of heart disease. Abdominal ultrasound may be useful for exploring underlying kidney disease.
Because the signs of feline hyperthyroidism can overlap with signs of kidney disease, liver disease, and cancer (especially intestinal lymphoma), it is important to perform the blood and urine diagnostics to confirm hyperthyroidism and to help rule out other conditions.
If concurrent heart disease is diagnosed, chest x-rays (thoracic radiography) and an ultrasound of the heart (echocardiography) may be useful in assessing the severity of heart disease. Abdominal ultrasound may be useful for exploring underlying kidney disease.
Feline hyperthyroidism has three treatment options: medication, surgery, or radioactive iodine therapy. In general, the treatment choice will depend on your cat’s age, condition, and presence of any concurrent disease.
Medication
Methimazole is an oral medication that reduces the production of thyroid hormone from the thyroid glands. This medication does not provide a cure for the disease, but allows either short-term or long-term control of hyperthyroidism. Methimazole is readily available and inexpensive. Some cats may experience side effects, including vomiting, anorexia, fever, anemia, and lethargy. Lifelong treatment, usually involving twice-daily oral dosage, will be required for most cats. Routine blood tests should be done periodically during treatment to evaluate the effectiveness of therapy, monitor kidney function, and look for side effects.
Surgical Treatment
Surgical removal of the thyroid glands is likely to produce a permanent cure in most cats and therefore eliminates the need for long-term medication. The surgery requires general anesthesia, and there are added risks if older cats have heart, kidney, or other problems that could increase the risk of surgical complications. A major risk associated with the surgical procedure is inadvertent damage to the parathyroid glands, which lie close to or within the thyroid glands, and are crucial in maintaining stable blood calcium levels. If these glands are damaged your cat will need to take an additional medication for the rest of his or her life.
Radioactive Iodine Therapy
Radioactive iodine therapy has become the treatment of choice for most cats with hyperthyroidism. Radioactive iodine is administered as an injection and is selectively absorbed by the thyroid gland. The low-dose radiation destroys the abnormal thyroid tissue but does not damage the surrounding tissues or the parathyroid glands. The majority of cats have normal hormone levels within one to two weeks of treatment.
The advantages of radioactive iodine therapy are that the procedure is curative, has no serious side effects, and does not require anesthesia. It involves the handling and injection of a radioactive substance that is only permitted at facilities specially licensed to use radioisotopes. The radioactivity carries no significant risk for the cat, but a treated cat has to remain hospitalized for several days until the radiation level has fallen to within acceptable limits. Because of strict treatment guidelines, most facilities will not allow visitors.
Radioactive iodine therapy is curative in approximately 95% of all hyperthyroid cases. For the few cats where hyperthyroidism persists, the treatment can be repeated. Rarely, a permanent reduction in thyroid hormone levels (hypothyroidism) occurs after radioactive iodine treatment. In these cases thyroid hormone supplementation may be required.
Medication
Methimazole is an oral medication that reduces the production of thyroid hormone from the thyroid glands. This medication does not provide a cure for the disease, but allows either short-term or long-term control of hyperthyroidism. Methimazole is readily available and inexpensive. Some cats may experience side effects, including vomiting, anorexia, fever, anemia, and lethargy. Lifelong treatment, usually involving twice-daily oral dosage, will be required for most cats. Routine blood tests should be done periodically during treatment to evaluate the effectiveness of therapy, monitor kidney function, and look for side effects.
Surgical Treatment
Surgical removal of the thyroid glands is likely to produce a permanent cure in most cats and therefore eliminates the need for long-term medication. The surgery requires general anesthesia, and there are added risks if older cats have heart, kidney, or other problems that could increase the risk of surgical complications. A major risk associated with the surgical procedure is inadvertent damage to the parathyroid glands, which lie close to or within the thyroid glands, and are crucial in maintaining stable blood calcium levels. If these glands are damaged your cat will need to take an additional medication for the rest of his or her life.
Radioactive Iodine Therapy
Radioactive iodine therapy has become the treatment of choice for most cats with hyperthyroidism. Radioactive iodine is administered as an injection and is selectively absorbed by the thyroid gland. The low-dose radiation destroys the abnormal thyroid tissue but does not damage the surrounding tissues or the parathyroid glands. The majority of cats have normal hormone levels within one to two weeks of treatment.
The advantages of radioactive iodine therapy are that the procedure is curative, has no serious side effects, and does not require anesthesia. It involves the handling and injection of a radioactive substance that is only permitted at facilities specially licensed to use radioisotopes. The radioactivity carries no significant risk for the cat, but a treated cat has to remain hospitalized for several days until the radiation level has fallen to within acceptable limits. Because of strict treatment guidelines, most facilities will not allow visitors.
Radioactive iodine therapy is curative in approximately 95% of all hyperthyroid cases. For the few cats where hyperthyroidism persists, the treatment can be repeated. Rarely, a permanent reduction in thyroid hormone levels (hypothyroidism) occurs after radioactive iodine treatment. In these cases thyroid hormone supplementation may be required.